Let me take a break from the story here to give a few definitions, as this was all pretty new to me I did some research of my own:
Insulinoma: A tumor of the beta cells in areas of the pancreas called the islets of Langerhans. Although not usually cancerous, such tumors may cause the body to make extra insulin and may lead to hypoglycemia, a blood glucose (sugar) level that is too low.
Hypoglycemia: Low blood sugar (glucose). When symptoms of hypoglycemia occur together with a documented blood glucose under 45 mg/dl, and the symptoms promptly resolve with the administration of glucose, the diagnosis of hypoglycemia can be made with some certainty. Hypoglycemia is only significant when it is associated with symptoms.
The symptoms may include anxiety, sweating, tremor, palpitations, nausea, and pallor. Hypoglycemia also starves the brain of glucose energy, which is essential for proper brain function. Lack of glucose energy to the brain can cause symptoms ranging from headache, mild confusion, and abnormal behavior, to loss of consciousness, seizure, and coma. Severe hypoglycemia can cause death.
The causes of hypoglycemia include drugs (such as insulin), liver disease, surgical absence of the stomach, tumors that release excess amounts of insulin, and pre-diabetes. In some patients, symptoms of hypoglycemia occur during fasting (fasting hypoglycemia). In others, symptoms of hypoglycemia occur after meals (reactive hypoglycemia).
Immediate treatment of severe hypoglycemia consists of administering large amounts of glucose, and repeating this treatment at intervals if the symptoms persist. Treatment must also be directed at the underlying cause. Patients with diabetes mellitus who develop low blood glucose from their medicines require medication adjustments. Treatment of reactive hypoglycemia consists of dietary measures, including fewer concentrated sweets and the ingestion of multiple small meals throughout the day.
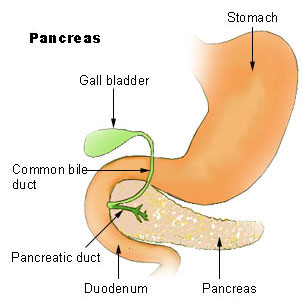
Pancreas: A fish-shaped spongy grayish-pink organ about 6 inches (15 cm) long that stretches across the back of the abdomen, behind the stomach. The head of the pancreas is on the right side of the abdomen and is connected to the duodenum (the first section of the small intestine). The narrow end of the pancreas, called the tail, extends to the left side of the body.
The pancreas makes pancreatic juices and hormones, including insulin. The pancreatic juices are enzymes that help digest food in the small intestine. Insulin controls the amount of sugar in the blood.
As pancreatic juices are made, they flow into the main pancreatic duct. This duct joins the common bile duct, which connects the pancreas to the liver and the gallbladder. The common bile duct, which carries bile (a fluid that helps digest fat), connects to the small intestine near the stomach.
The pancreas is thus a compound gland. It is "compound" in the sense that it is composed of both exocrine and endocrine tissues. The exocrine function of the pancreas involves the synthesis and secretion of pancreatic juices. The endocrine function resides in the million or so cellular islands (the islets of Langerhans) embedded between the exocrine units of the pancreas. Beta cells of the islands secrete insulin, which helps control carbohydrate metabolism. Alpha cells of the islets secrete glucagon that counters the action of insulin.
Tumor: An abnormal mass of tissue. Tumors are a classic sign of inflammation, and can be benign or malignant (cancerous). There are dozens of different types of tumors. Their names usually reflect the kind of tissue they arise in, and may also tell you something about their shape or how they grow. For example, a medulloblastoma is a tumor that arises from embryonic cells (a blastoma) in the inner part of the brain (the medulla). Diagnosis depends on the type and location of the tumor. Tumor marker tests and imaging may be used; some tumors can be seen (for example, tumors on the exterior of the skin) or felt (palpated with the hands).
Treatment is also specific to the location and type of the tumor. Benign tumors can sometimes simply be ignored, or they may be reduced in size (debulked) or removed entirely via surgery. For cancerous tumors, options include chemotherapy, radiation, and surgery. See also blastoma, carcinoembryonic antigen test, desmoid tumor, ear tumor, epidermoid carcinoma, epithelial carcinoma, esophageal cancer, syringoma, fibroid, tumor marker.
More on insulinomas:
Insulinoma is a tumor of the pancreas that produces excessive amounts of insulin. Insulinomas are more common in women. The tumors are usually small (less than 2cm) and more than 90% of all insulinomas are benign (non-cancerous).
How is diagnosis made:
The diagnosis is made by simultaneous measurements of blood sugar and insulin levels in the blood. A low blood sugar with a high insulin level confirms the diagnosis. Once the diagnosis made based on the biochemical analysis then the physician will perform further studies to detect the tumor in the pancreas.
Since most of these tumors are small, detection of the tumor in the pancreas may be difficult. Some of the studies that are performed to detect the tumor include a detailed CT scan, MRI, octreotide scan, and an endoscopic ultrasound.
An experienced surgeon often detects these tumors even where they are not seen on radiological testing prior to surgery. Imaging the pancreas during the surgery directly with an ultrasound detects the majority of these tumors.
Treatment:
Insulinoma is a benign tumor of the pancreas in 90% of patients and removal of the tumor cures the patient of the symptoms. Surgical removal of the tumor is the treatment of choice. More than 90% of patients will not require any further treatment after removal of the tumor. The operations that are usually performed for removing the insulinoma include:
Enucleation: In this procedure the surgeon removes only the tumor preserving the rest of the pancreas. Since insulinomas usually occur on the surface of the pancreas and are covered by a capsule, they can be completely removed without having to remove any of the surrounding pancreas. At USC we have developed a laparoscopic procedure for enucleation of pancreatic insulinoma.The recurrence rate after enucleation of the insulinoma is very low and this is the treatment of choice if it is technically possible to perform this operation.
Pancreatic resection (removal): Less commonly the surgeon may remove part of the pancreas where the tumor is located by utilizing operative procedures such as a distal pancreatectomy or a Whipple operation. These operations are performed as an exception rather than commonly since the vast majority of the tumors can be removed with enucleation.
Laparoscopic operations: At USC we offer a laparoscopic procedure for removing pancreatic insulinoma. The operation of enucleation of the insulinoma is performed laparoscopically. With laparoscopic surgery the post-operative recovery period and amount of pain is reduced, hospital stay is shorter and patients are able to return to their normal activity much faster.
Frequency:
In the US: Insulinomas are the most common pancreatic endocrine tumor. The incidence is about 1 case per 250,000 patient-years or 1-4 per million people. Approximately 50% of islet cell tumors are insulinomas. (Thirty percent are gastrinomas; 10-15%, VIPomas; and 5-10%, other tumor types, including glucagonomas and somatostatinomas.)
Internationally: Exact data are not available. One source from Northern Ireland reported an annual incidence of 1 case per million persons. This report may be an underestimate.
Mortality/Morbidity: The postoperative morbidity rate in a recently published series was 14%, mainly due to local complications, such as fistula formation after pancreatic resections. The postoperative mortality rate in another series of 117 insulinoma patients was 7.7%.
The median survival in metastatic disease to the liver ranges from 16-26 months.
Sex: The male-to-female ratio is 2:3.
Age: The median age at diagnosis is about 50 years, except in insulinoma patients with MEN 1, in whom the median age is the mid 20s.
In one series, patients with benign disease were younger (mean age of 38 y) than those with metastases (mean age of 52 y).
Insulinoma: A tumor of the beta cells in areas of the pancreas called the islets of Langerhans. Although not usually cancerous, such tumors may cause the body to make extra insulin and may lead to hypoglycemia, a blood glucose (sugar) level that is too low.
Hypoglycemia: Low blood sugar (glucose). When symptoms of hypoglycemia occur together with a documented blood glucose under 45 mg/dl, and the symptoms promptly resolve with the administration of glucose, the diagnosis of hypoglycemia can be made with some certainty. Hypoglycemia is only significant when it is associated with symptoms.
The symptoms may include anxiety, sweating, tremor, palpitations, nausea, and pallor. Hypoglycemia also starves the brain of glucose energy, which is essential for proper brain function. Lack of glucose energy to the brain can cause symptoms ranging from headache, mild confusion, and abnormal behavior, to loss of consciousness, seizure, and coma. Severe hypoglycemia can cause death.
The causes of hypoglycemia include drugs (such as insulin), liver disease, surgical absence of the stomach, tumors that release excess amounts of insulin, and pre-diabetes. In some patients, symptoms of hypoglycemia occur during fasting (fasting hypoglycemia). In others, symptoms of hypoglycemia occur after meals (reactive hypoglycemia).
Immediate treatment of severe hypoglycemia consists of administering large amounts of glucose, and repeating this treatment at intervals if the symptoms persist. Treatment must also be directed at the underlying cause. Patients with diabetes mellitus who develop low blood glucose from their medicines require medication adjustments. Treatment of reactive hypoglycemia consists of dietary measures, including fewer concentrated sweets and the ingestion of multiple small meals throughout the day.
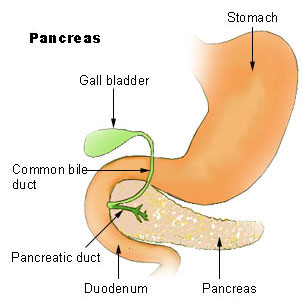
Pancreas: A fish-shaped spongy grayish-pink organ about 6 inches (15 cm) long that stretches across the back of the abdomen, behind the stomach. The head of the pancreas is on the right side of the abdomen and is connected to the duodenum (the first section of the small intestine). The narrow end of the pancreas, called the tail, extends to the left side of the body.
The pancreas makes pancreatic juices and hormones, including insulin. The pancreatic juices are enzymes that help digest food in the small intestine. Insulin controls the amount of sugar in the blood.
As pancreatic juices are made, they flow into the main pancreatic duct. This duct joins the common bile duct, which connects the pancreas to the liver and the gallbladder. The common bile duct, which carries bile (a fluid that helps digest fat), connects to the small intestine near the stomach.
The pancreas is thus a compound gland. It is "compound" in the sense that it is composed of both exocrine and endocrine tissues. The exocrine function of the pancreas involves the synthesis and secretion of pancreatic juices. The endocrine function resides in the million or so cellular islands (the islets of Langerhans) embedded between the exocrine units of the pancreas. Beta cells of the islands secrete insulin, which helps control carbohydrate metabolism. Alpha cells of the islets secrete glucagon that counters the action of insulin.
Tumor: An abnormal mass of tissue. Tumors are a classic sign of inflammation, and can be benign or malignant (cancerous). There are dozens of different types of tumors. Their names usually reflect the kind of tissue they arise in, and may also tell you something about their shape or how they grow. For example, a medulloblastoma is a tumor that arises from embryonic cells (a blastoma) in the inner part of the brain (the medulla). Diagnosis depends on the type and location of the tumor. Tumor marker tests and imaging may be used; some tumors can be seen (for example, tumors on the exterior of the skin) or felt (palpated with the hands).
Treatment is also specific to the location and type of the tumor. Benign tumors can sometimes simply be ignored, or they may be reduced in size (debulked) or removed entirely via surgery. For cancerous tumors, options include chemotherapy, radiation, and surgery. See also blastoma, carcinoembryonic antigen test, desmoid tumor, ear tumor, epidermoid carcinoma, epithelial carcinoma, esophageal cancer, syringoma, fibroid, tumor marker.
More on insulinomas:
Insulinoma is a tumor of the pancreas that produces excessive amounts of insulin. Insulinomas are more common in women. The tumors are usually small (less than 2cm) and more than 90% of all insulinomas are benign (non-cancerous).
How is diagnosis made:
The diagnosis is made by simultaneous measurements of blood sugar and insulin levels in the blood. A low blood sugar with a high insulin level confirms the diagnosis. Once the diagnosis made based on the biochemical analysis then the physician will perform further studies to detect the tumor in the pancreas.
Since most of these tumors are small, detection of the tumor in the pancreas may be difficult. Some of the studies that are performed to detect the tumor include a detailed CT scan, MRI, octreotide scan, and an endoscopic ultrasound.
An experienced surgeon often detects these tumors even where they are not seen on radiological testing prior to surgery. Imaging the pancreas during the surgery directly with an ultrasound detects the majority of these tumors.
Treatment:
Insulinoma is a benign tumor of the pancreas in 90% of patients and removal of the tumor cures the patient of the symptoms. Surgical removal of the tumor is the treatment of choice. More than 90% of patients will not require any further treatment after removal of the tumor. The operations that are usually performed for removing the insulinoma include:
Enucleation: In this procedure the surgeon removes only the tumor preserving the rest of the pancreas. Since insulinomas usually occur on the surface of the pancreas and are covered by a capsule, they can be completely removed without having to remove any of the surrounding pancreas. At USC we have developed a laparoscopic procedure for enucleation of pancreatic insulinoma.The recurrence rate after enucleation of the insulinoma is very low and this is the treatment of choice if it is technically possible to perform this operation.
Pancreatic resection (removal): Less commonly the surgeon may remove part of the pancreas where the tumor is located by utilizing operative procedures such as a distal pancreatectomy or a Whipple operation. These operations are performed as an exception rather than commonly since the vast majority of the tumors can be removed with enucleation.
Laparoscopic operations: At USC we offer a laparoscopic procedure for removing pancreatic insulinoma. The operation of enucleation of the insulinoma is performed laparoscopically. With laparoscopic surgery the post-operative recovery period and amount of pain is reduced, hospital stay is shorter and patients are able to return to their normal activity much faster.
Frequency:
In the US: Insulinomas are the most common pancreatic endocrine tumor. The incidence is about 1 case per 250,000 patient-years or 1-4 per million people. Approximately 50% of islet cell tumors are insulinomas. (Thirty percent are gastrinomas; 10-15%, VIPomas; and 5-10%, other tumor types, including glucagonomas and somatostatinomas.)
Internationally: Exact data are not available. One source from Northern Ireland reported an annual incidence of 1 case per million persons. This report may be an underestimate.
Mortality/Morbidity: The postoperative morbidity rate in a recently published series was 14%, mainly due to local complications, such as fistula formation after pancreatic resections. The postoperative mortality rate in another series of 117 insulinoma patients was 7.7%.
The median survival in metastatic disease to the liver ranges from 16-26 months.
Sex: The male-to-female ratio is 2:3.
Age: The median age at diagnosis is about 50 years, except in insulinoma patients with MEN 1, in whom the median age is the mid 20s.
In one series, patients with benign disease were younger (mean age of 38 y) than those with metastases (mean age of 52 y).
Comments
i hope there are many many more survivors out there.